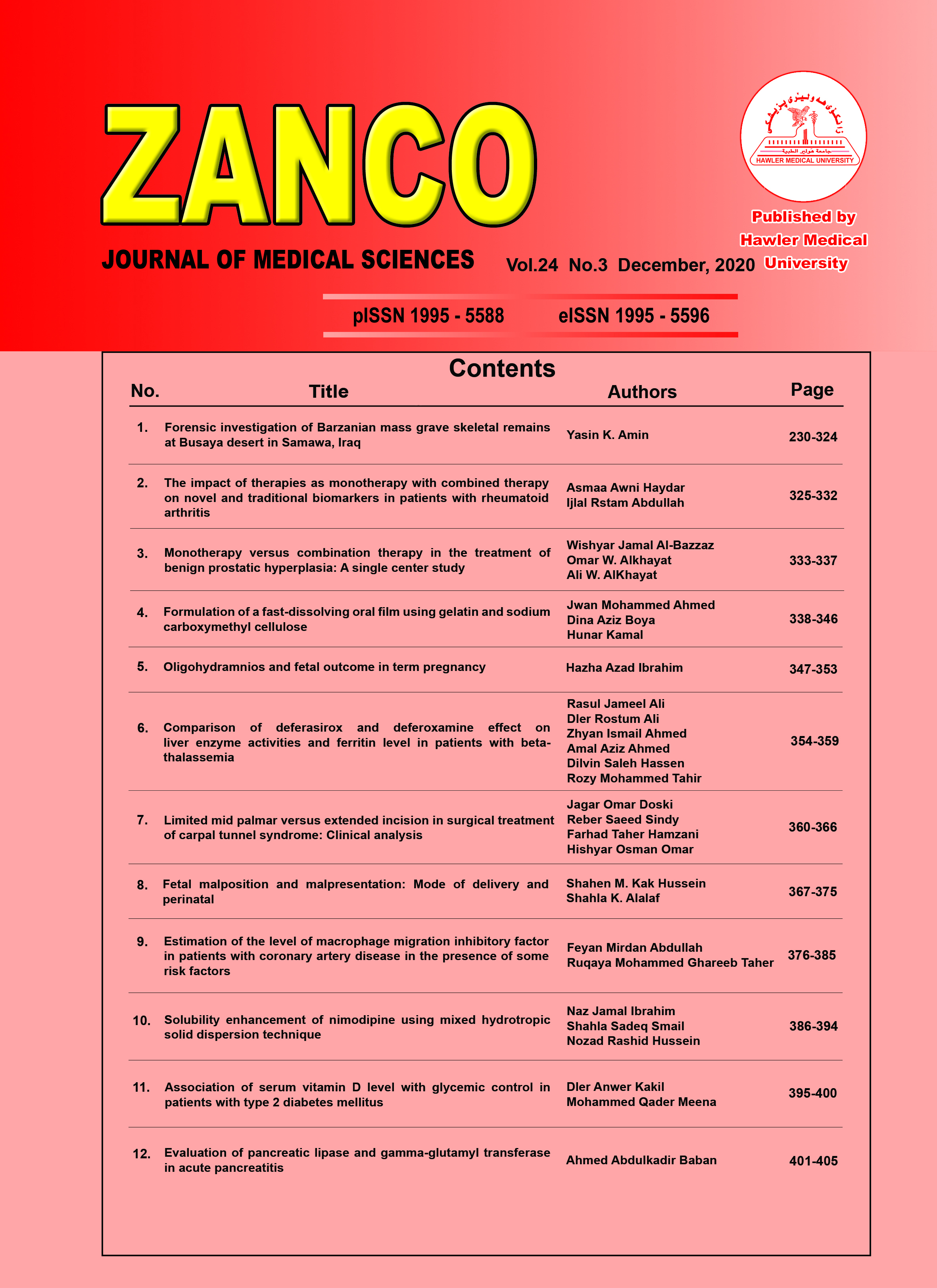
Fetal malposition and malpresentation: Mode of delivery and perinatal outcomes at Maternity Teaching Hospital in Erbil city
Copyright (c) 2020 Shahen M. Kak Hussein, Shahla K. Alalaf (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- Articles
- Submited: January 13, 2021
-
Published: December 24, 2020
Abstract
Background and objective: Delivering a malpositioned and malpresenting fetus remains uncertainty, despite advances in obstetric practice. This study aimed to determine the mode of delivery and neonatal outcome in cases of fetal malposition and malpresentation.
Results: The total rate of malposition and malpresentation was 4.8%. Most women (87.3%) delivered by cesarean section, 25% of the neonates were admitted to the neonatal intensive care unit, where 69.3% of these infants stayed for seven days. There were three early neonatal deaths (1.0%), all of them were in occipito-posterior, or occipito-transverse position and were delivered abdominally. Among occipito-posterior and occipito-transverse deliveries, 2.2% ended with the death of the fetus (P = 0.360). An Apgar score of 7 was recorded after 5 minutes for 97.7% of the infants. Around 11% of the women had postpartum hemorrhage.
Conclusion: Fetal malpresentation and malposition are not uncommon during labor, and most cases are delivered by cesarean section. Neonatal morbidity and mortality are dependent on the type of presentation and the mode of delivery.
Metrics
References
- Stitel LM, Gherman BR. Labor with abnormal presentation and position. Obstet Gynecol Clin N Am 2005; 32:165–79.
- Pilliod RA, Caughey A. Fetal malpresentation and malposition: diagnosis and management. Obstet Gynecol Clin North Am 2017; 44:631–43.
- Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C, editors. Williamsobstetrics. 23rded. New York: McGraw-Hill Companies, Inc.; 2010.
- Caughey AB, Sharshiner R, Cheng YW. Fetal malposition: Impact and management. Clin Obstet Gynecol 2015; 58:241–55.
- Ali R, Abrar A. Transverse lie; predisposing factors, maternal and perinatal outcome. Professional Med J 2011; 18:208–11.
- Bashiri A, Burstein E, Bar-David J, Levy A, Mazor M. Face and brow presentation: independent risk factors. J Matern Fetal Neonatal Med 2008; 21:357–60.
- Zayed F, Amarin Z, Obeidat B, Obeidat N, Alchalabi H, LataifehI. Face and brow presentation in northern Jordan, over a decade of experience. Arch Gynecol Obstet 2008; 278:427–30.
- Cheng YV, Shaffer BL, Caughey AB. The association between persistent occiput posterior position and neonatal outcomes. Obstet Gynecol 2006; 107:837–44.
- Senécal J, Xiong XU, Fraser WD, Pushing Early Or Pushing Late with Epidural Study Group. Effect of fetal position on second-stage duration and labor outcome. Obstet Gynecol 2005; 105:763–72.
- Ponkey SE, Cohen AP, Heffner LJ, Lieberman E.Persistent fetal occiput posterior position: obstetric outcomes. Obstet Gynecol 2003; 101:915–20.
- El-Hamamy E, Arulkumaran S. Poor progress of labour. Curr Opin Gynecol Obstet 2005; 15:1–8.
- Gardberg M, Leonova Y, Laakkonen E. Malpresentations – impact on mode of delivery. Acta Obstet Gynecol Scand 2011; 90:540–4.
- Dahiya K, Khosla AH, Sangwan K. Transverse lie in labour: Alternative options. Trop Doctor 2004; 34:43–4.
- Shaffer BL, Cheng YW, Vargas JE, Laros RK, Caughey AB. Face presentation: Predictors and delivery route. Am J Obstet Gynecol 2006; 194:e10–2.
- LeRay C, Carayol M, Jaquemin S, Mignon A, Cabrol D, Goffinet F, et al. Is epidural analgesia a risk factor for occiput posterior or transverse positions during labour? Eur J Obstet Gynecol Reprod Biol 2005; 123:22–6.
- Andrews CM, Andrews EC. Physical theory as the basis for successful rotation of fetal malpositions and conversion of fetal malpresentations. Biological Research for Nursing 2004; 6:126–40.
- World Health Organization. Neonatal and perinatal mortality: country, regional and global estimates. Geneva: World Health Organization; 2006. (Accessed July 24, 2019, at https://apps.who.int/iris/handle/10665/43444).
- Committee on Obstetric Practice American Academy of Pediatrics—Committee on Fetus and Newborn. Committee opinion No. 644: the Apgar score. Obstet Gynecol 2015;126:252–5.
- Say L, Chou D, Gemmill A, Tuncalp O, Moller AB, Daniels J, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health 2014; 2:e323–33.
- ACOG. ACOG committee opinion: Mode of term singleton breech delivery. Int J Gynaecol Obstet 2002; 77:65–6.
- ACOG. ACOG committee opinion No. 340. Mode of term singleton breech delivery. Obstet Gynecol 2006; 108:235–7.
- ACOG. Practice bulletin No. 106: intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 2009; 114:192–202.
- Alexandersson O, Bixo M, Högberg U. Evidence-based changes in term breech delivery practice in Sweden. Acta Obstet Gynecol Scand 2005; 84:584–7.
- Rietberg CC, Elferink-Stinkens PM, Visser G. The effect of the Term Breech Trial on medical intervention behaviour and neonatal outcome in The Netherlands: an analysis of 35,453 term breech infants. BJOG 2005; 112:205–9.
- HartnackTharin JE, Rasmussen S, Krebs L. Consequences of the Term Breech Trial in Denmark. Acta Obstet Gynecol Scand 2011; 90:767–71.
- Kotaska A. Commentary: routine cesarean section for breech: the unmeasured cost. Birth 2011; 38:162–4.
- Lyons J, Pressey T, Bartholomew S, Liu S, Liston RM, Joseph KS. Delivery of breech presentation at term gestation in Canada, 2003–2011. Obstet Gynecol 2015; 125:1153–61.
- Heino A, Vuori E, Gissler M. Perinatal statistics - births, deliveries and newborns 2016. (Accessed June 15, 2019, at http://urn.fi/URN:NBN:Fi-fe2017103150386).
- Antenatal obstetrics complications. In Baker PN, editor. Obstetrics by ten teachers’ 18thed.London: Book Power; 2006. P. 125–45.