Copyright and Licensing:
Copyright (c) 2014 Omar Ameen Saeed, Salahaddin H. Abdulqadir (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- Articles
- Submited: September 26, 2018
-
Published: April 1, 2014
Abstract
Background and objective: Tibial diaphyseal fracture is of two types, closed fracture, in which the skin is intact and open fracture in which the skin is injured. An open fracture is a type of fracture in which a break in the skin and underlying soft tissues communicates with the fracture and its haematoma .i.e. the fracture and its haematoma communicates with external environment. Our aim is to evaluate the treatment outcome of this structured protocol in terms of soft tissue injury healing and effective fracture stabilization by POP and external fixation, and to detect if there is any difference in time needed for union in both methods. Methods: This is a comparative study done in Emergency hospital in Erbil – Kurdistan region, for management of open tibial diaphyseal fractures caused by gunshot injuries. The study included 50 patients of 18 to 65 years old. Patients were divided into two groups after debridment according to methods of treatment; group 1 was managed by POP, group 2 was managed by external fixation. The patients recruited and treated over 11 month period (August 2007 to June 2008). Results: The study included 50 patients; 44 males (88%) and six females (12%). Their ages ranged between 18 years and 65 years with the mean age of 27.46 years. Patients divided into three groups according to Gustilo classification: GI included 8 patients (16%), GII included 34 patients (68%) and GIII included 8 patients (2A, 6B) (16%). There was significant difference between immobilization of open tibial diaphyseal fractures by pop and external fixation (P=0.001). Conclusion: There will be delay union of the fractures when immobilized by external fixation. It is better to remove external fixature after 6 weeks and replace it by another method of immobilization of the fracture. Treatment of type III fracture is very difficult and needs long time, usually more than one year.Metrics
Metrics Loading ...
References
- Shanker A, Ratra GS, Bhartendra J. Management of open fractures. Journal of Orthopaedics 2007; 4(1):e18.
- Oscar P, Hampton JR. Orthopedic surgery in the Mediterranean theater of operations. Washington: US Government Printing Office; 1957.
- Rowley D L. War wounds with fractures: A guide to surgical management. Geneva: ICRC: 1996.
- Bowyer G. Débridement of extremity war wounds. J Acad Orthop Surg 2006; 14(10):S52-6.
- Chapman MW, Szabo RM, Richard M. Chapmans orthopaedic surgery. 3rd edition. Philadelphia, Pa: Lippincott, Williams & Wilkins: 2000.
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of open fractures of long bones. J Bone Joint Surg Am 1976; 58:453-8.
- Sam W, John N. Essentials of orthopaedic surgery. 3rd edition. New York: Springer Science and Business Media, LLC; 2007.
- Warwick SL, David J, Selvadurai N. Apleys System of orthopedics and fractures, 8th edition. London: Arnold; 2001. p. 561.
- Philip AF. Early management of open tibial fractures in Benin city. Journal of Medicine and Biomedical Research 2006; 5(12):33-9
- Minoo P. Tibia fractures. Available from https:// www.emedicine.com/orthoped/topic 336.htm
- Charalampos ZG, Randall ME, Levins L, Patzakis MJ. Management of open fracture and subsequent complication. Journal of Bone and Joint Surgery (American) 2007; 89:884-95.
- David BE, Neumann R D. Orthopedic secrets. 2nd edition. Philadelphia: Hanley & Belfus INC; 1999. p. 327.
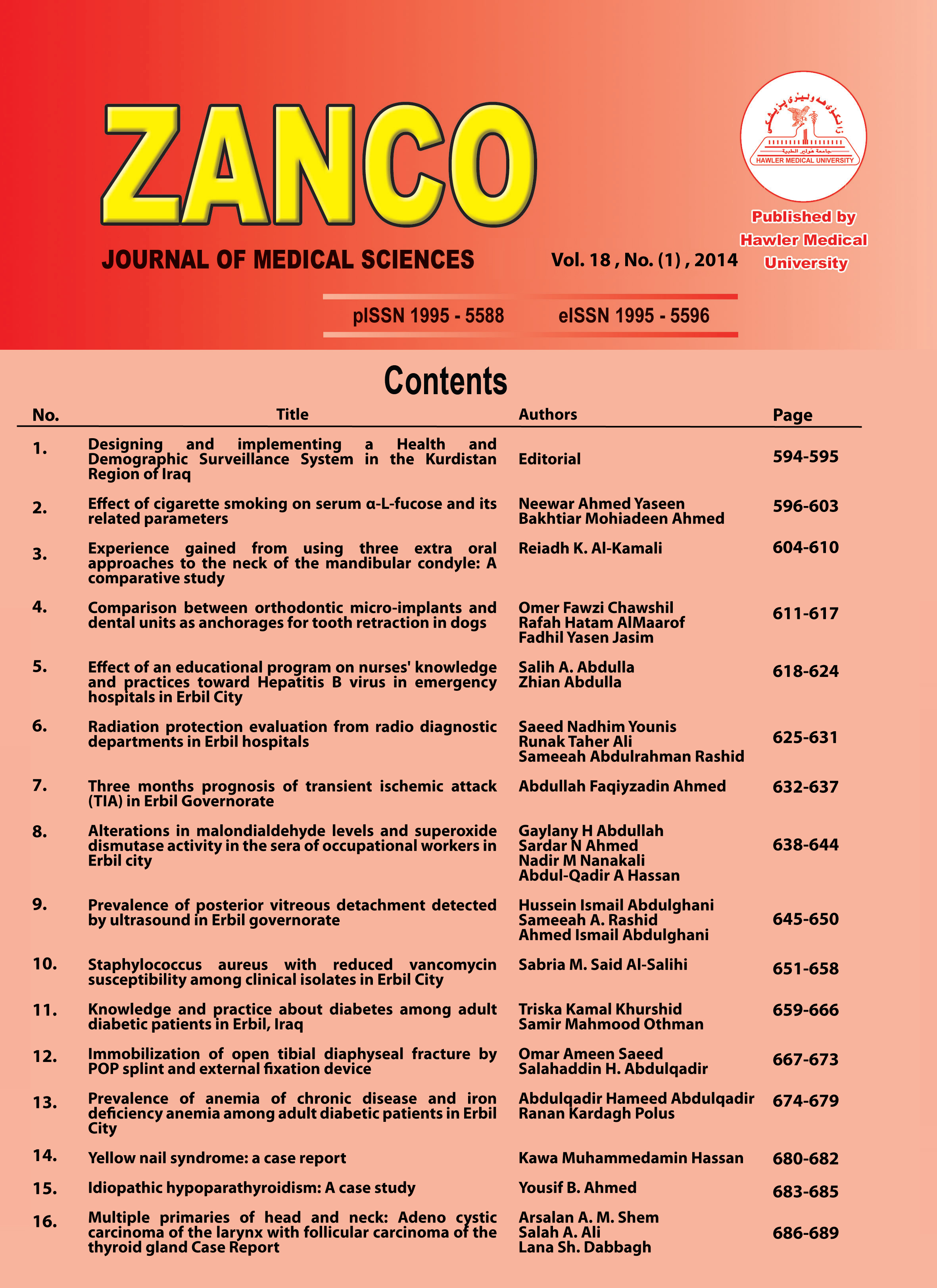
How to Cite
Saeed, O. A., & Abdulqadir, S. H. (2014). Immobilization of open tibial diaphyseal fracture by POP splint and external fixation device. Zanco Journal of Medical Sciences (Zanco J Med Sci), 18(1), 667_673. https://doi.org/10.15218/zjms.2014.0012