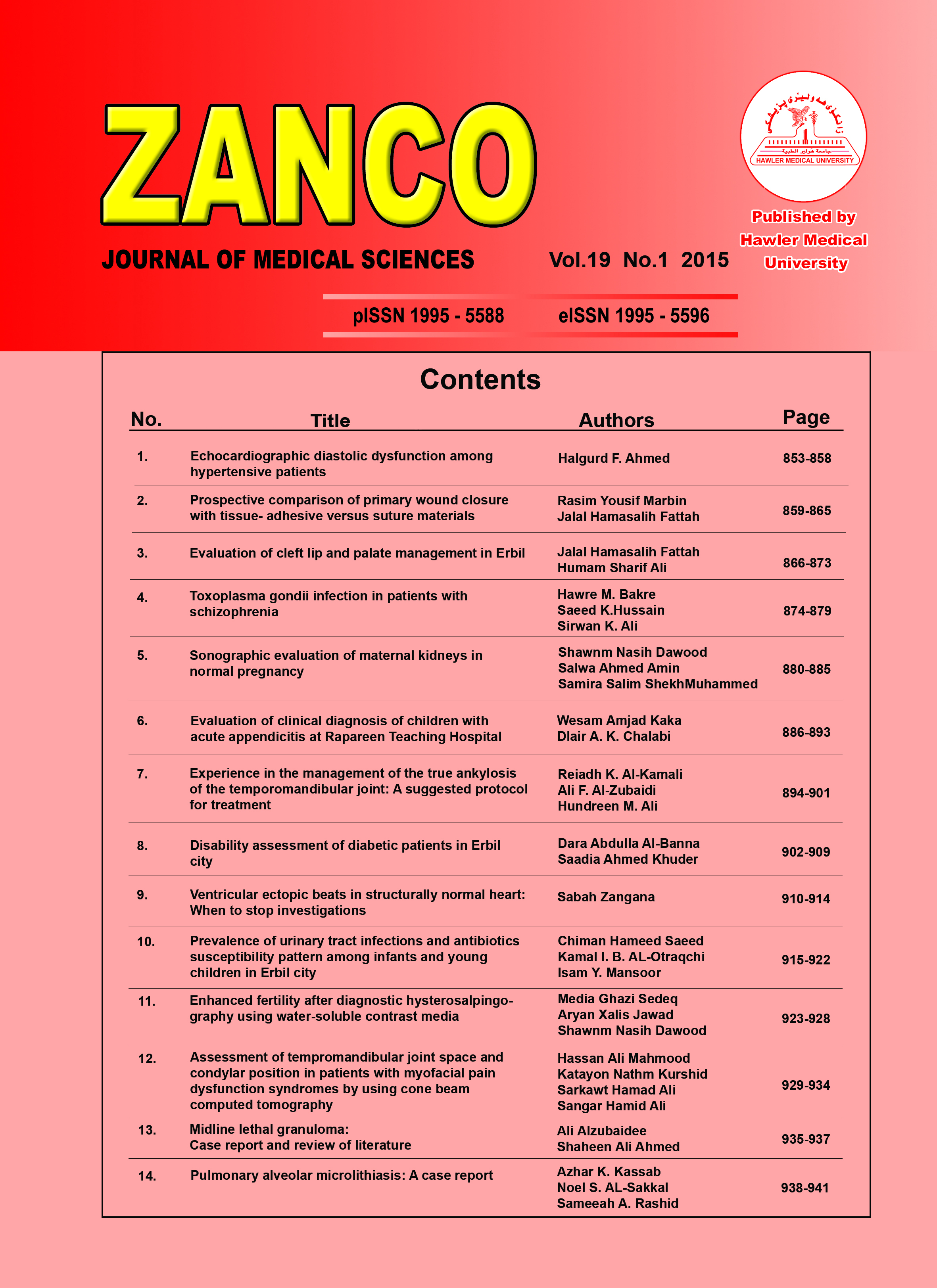
Assessment of tempromandibular joint space and condylar position in patients with myofacial pain dysfunction syndromes by using cone beam computed tomography
Copyright and Licensing:
Copyright (c) 2015 Hassan Ali Mahmood, Katayon Nathm Kurshid, Sarkawt Hamad Ali, Sangar Hamid Ali (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- Articles
- Submited: September 24, 2018
-
Published: April 1, 2015
Abstract
Background and objectives: Joint space assessment and condylar relation in the glenoid fossa is considered as integral component of the clinical assessment of the patient with tempromandibular joint disorder. Any variant from normal tempromandibular joint may affect the diagnosis and management of the case. Methods: Thirty patients with unilateral myofacial pain dysfunction syndrome were included in this study (14 male and 16 female). Joint space analysis was performed by cone beam computed tomography for all patients. Analysis of data for joint spaces (anterior, middle, posterior, medial and lateral) was performed by using t-test. Results: The joint spaces and condyle positions in anterior, superior and posterior regions showed less joint space and statistically significant difference (P <0.05) from same joint space of normal side. No statistically significant differences were found in space value between middle and lateral condylar space of the diseased side and normal side of the patient. The joint spaces in normal sides were between 2 to 3.2 mm. Age and gender variations showed no statistical differences. Conclusion: The use of cone beam computed tomography for examination of tempromandibular joint space in patients with myofacial pain dysfunction syndrome give a good diagnostic criteria for affected side.Metrics
Metrics Loading ...
References
- White S, Pharoah M. Oral Radiology Principles and interpretation. 1st ed. St. Louis, Mo.: Mosby/Elsevier; 1987. P. 654-5.
- Cawson R, Odell E. Cawson's essentials of oral pathology and oral medicine.1st ed. Edinburgh: Churchill Livingstone; 2008. P.192-3.
- Burket L, Greenberg M, Glick M, Ship J. Burket's oral medicine. 1st ed. Hamilton, Ont.: BC Decker; 2008. P. 223-43.
- Weinberg L. The role of stress, occlusion, and condyle position in TMJ dysfunction-pain. J Prosth Dentis 1983; 49(4):532-45.
- Field E, Longman L, Tyldesley W. Tyldesley's Oral medicine. 1st ed. Oxford: Oxford University Press; 2003. P.196-7.
- Palomo L, Palimo J. Cone beam Computed Tomography for diagnosis & treatment planning in trauma cases. J Clin Dentis 2009; 53:717-27.
- Chin L, Aker F, Zarrinnia K. The visco elastic properties of the human tempromandibular joint disc. J Oral Maxillofac Surg 1996; 54:315-8.
- Okeson J. Management of tempromandibular disorders and occlusion. 1st ed. St. Louis, Mo.: Mosby; 2003. P.228-9.
- Setton A, Zho W, Mow C. The Biphasic poro visco elastic behavior of articular cartilage: Role of the serface zone in governing the compressive behavior. J Biomech 1993; 26(4-5):581-92.
- Wang R, Max C, Zhang W, Liu D. Investigation of tempromandibular Joint space of healthy adults by using cone beam computed tomography. Dent Research J 2007; 39(5):503-6.
- Fushima K, Ballo L, Krebs M, Palla S. Analysis of the TMJ intra articular space variation: A non-invasive insight during mastication. Med Eng physic 2003; 25:181-90.
- Bhuvana K, Mamatha N , Kumar V. Review Practice Guidelines of TMJ imaging by CBCT. J Oral Maxillofac Radiol 2013; 3(1):80-3.
- Al-Ani Z ,Gray R , Stephen j,Philip D, and Annemarie G. Stabilzation splint therapy for the treatment-tempromandibular myofascial pain: Asystematic Review. JDent Educ 2005; 62(11):1242-50.
- Dalili Z, Khaki N, Kia S, Salamat F. Assessing joint space and condylar position in the people with normal function of temporomandibular joint with cone-beam computed tomography. Dent Research J 2012; 9(5):607-8.
- S"umb"ull"u M, Cauglayan F, Akg"ul H, Yilmaz A. Radiological examination of the articular eminence morphology using cone beam CT. Dent Maxillofac Radiol 2012; 41(3):234-6.
- Mirach A, Mukherji S. Cone beam CT of the head & neck , part 2 : clinical applications Am J Neuroradiol 2009; 30:1285-92.
- Scarfe W, Farman A, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Canad Dent Assoc 2006; 72(1):573-6.
- White S, Pharoah M. Oral radiology. 1st ed. St. Louis, Mo.: Mosby/Elsevier; 2009. P. 655-7.
- Petersson A. what you can and can't see in TMJ imaging an over view related the RDL /TMD diagnostic system. J Oral Rehab 2010; 37: 771-8.
How to Cite
Mahmood, H. A., Kurshid, K. N., Ali, S. H., & Ali, S. H. (2015). Assessment of tempromandibular joint space and condylar position in patients with myofacial pain dysfunction syndromes by using cone beam computed tomography. Zanco Journal of Medical Sciences (Zanco J Med Sci), 19(1), 929_934. https://doi.org/10.15218/zjms.2015.0014