Copyright and Licensing:
Copyright (c) 2015 Hawre M. Bakre, Saeed K. Hussain, Sirwan K. Ali (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
- Articles
- Submited: September 18, 2018
-
Published: April 1, 2015
Abstract
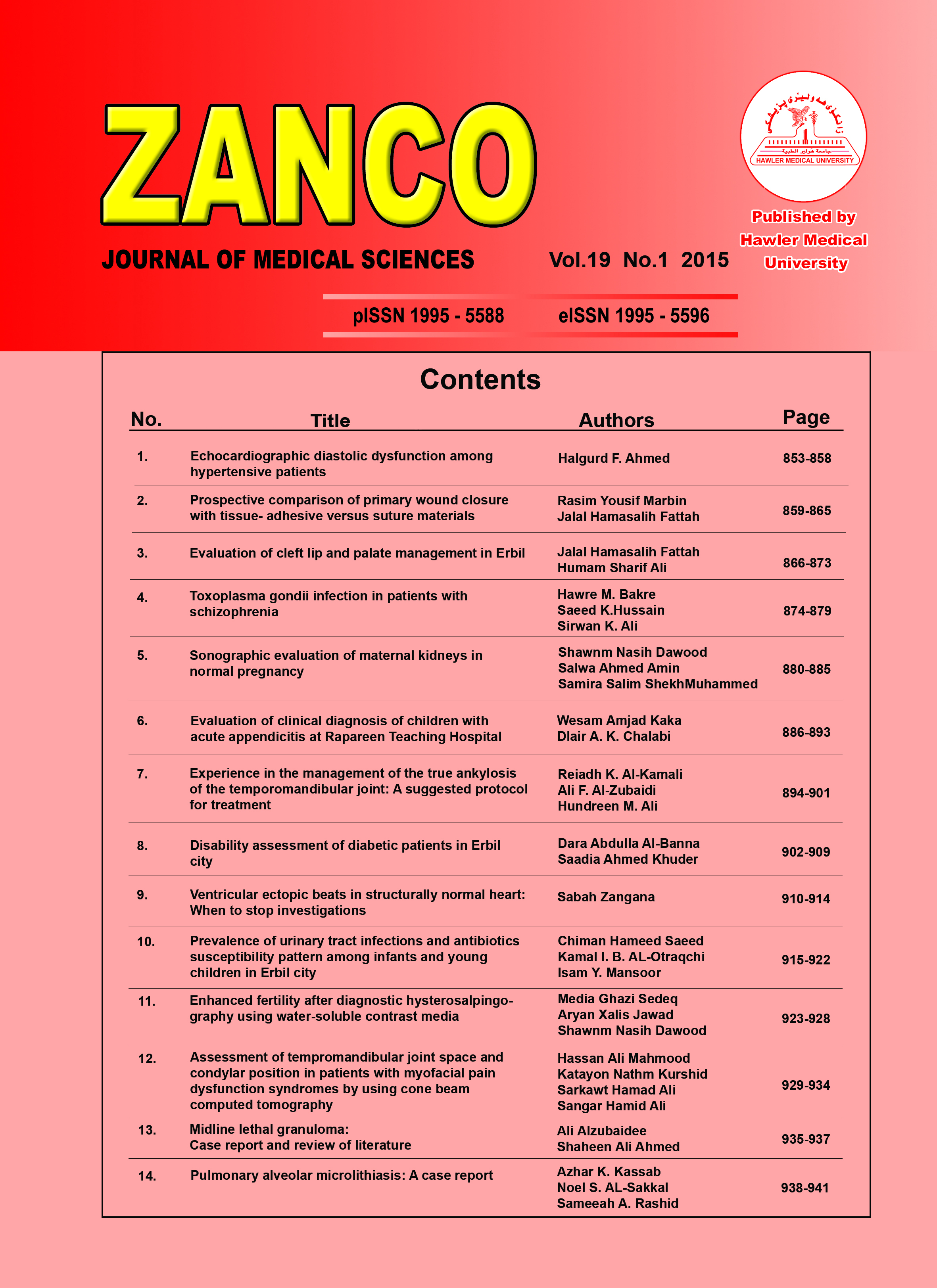
Background and Objectives: Schizophrenia is a complex chronic neuropsychiatric disease of the central nervous system, believed to have multiple etiologies. Toxoplasma gondii has emerged as an interesting candidate as a possible cause of some cases of schizophrenia. As there is scarce information about the seroprevalence of T. gondii infection in psychiatric patients in Erbil; we investigated the seroprevalence of T.gondii in schizophrenic patients and compared with that obtained from control individuals in Erbil correlated with inflammatory marker C-reactive protein. Method: This case control study included 93 schizophrenic patients seeking medical advice at Hawler Psychiatric Hospital and private clinics with 93 non psychiatric control were screened for the presence of anti-toxoplasma IgG, IgM (by ELISA test) and C-reactive protein using qualitative methods. A questionnaire was used to collect socio-demographic and behavioral data among the respondents. Results: In chronic cases anti-Toxoplasma gondii IgG antibodies were seropositive in 30/93 (32.3%) of the schizophrenic patients and 4/93(4.3%) of control (P <0.001). The seropositive rate of IgM antibodies was 9.7% and 1.1% among schizophrenic patients and control, respectively (P = 0.006). The result of C-reactive protein positivity among patients and control was 23.6% and 3.22%, respectively (P <0.001). Conclusion: Our results delineate that association might exist between Toxoplasma gondii infection and schizophrenia etiologyMetrics
Metrics Loading ...
References
- Juanah L Y, Jalaludin J, Osman M, Osman ZJ. Seroprevalence of Toxoplasma gondii among schizophrenics at hospital kajang. Am J Infec Dis 2013; 9 (1):11-6.
- Alvarado-Esquivel C, Estrada-Martinez S, Pizrro-Villalobos H, Arce-Quinones M. Seroepidemiology of Toxoplasma gondii infection in general population in a northern Mexican city. J Parasitol 2011; 97:40-3.
- Daryani A, Sharif M, Hosseini S H, Karimi SA, Gholami S. Serological survey of Toxoplasma gondii in schizophrenia patients referred to psychiatric hospital Sari city. Iran Tropical Biomedicine 2010; 27(3):476-82.
- Dubey JP, Jones JL. Toxoplasma gondii infection in humans and animals in the United States. Int J Parasitol 2008; 38:1257-78.
- Jones JL, Kruszon-Moran D, Wilson M, McQuillan G, Navin T, and McAuley JB. Toxoplasma gondii infection in the United States: seroprevalence and risk factors. Am J Epidemiol 2001; 154:57-65.
- Carruthers VB, Suzuki Y.Toxoplasma gondii infection on the brain. Schizophr Bull 2007; 33:745-51.
- Holiman RE. Toxoplasmosis, behavior and personality. J Infect Dis 1997; 35:105-10.
- Torrey EF, Yolken, RH. Toxoplasma gondii and schizophrenia. Emerg. Infect Dis 2003; 9:1375-80.
- Gaskell EA, Smith JE, Pinney JW, Westhead DR, McConkey GA. A unique dual activity amino acid Mahmoud hydroxylase in Toxoplasma gondii. Plos One 2009; 4: e4801. 161–72.
- Mahmoud SS, Hasan MS. Seroprevalence of toxoplasmosis among Schizophrenic patients. Yemeni J Med Sci 2009; 1(3):67–773
- Webster JP, McConkey GA. Toxoplasma gondii-altered host behaviour: clues as to mechanism of action. Folia Parasitologica Praha 2010; 57:95-104
- Flegr J. Effects of Toxoplasma gondii on human behavior. Schizophr Bull 2007: 33:757-60.
- Novotná M, Hanušová J, Klose J, Preiss M, Havlicek J, Roubalova K, et al. Probable neuroimmunological link between Toxoplasma and cytomegalovirus infections and personality changes in the human host. BMC Infect Dis 2005; 5:54.
- Hodková H, Kodym P, Flegr J. Poorer results of mice with latent toxoplasmosis in learning tests: impaired learning processes or the novelty discrimination mechanism. Parasite 2007; 134:1229-337.
- Mortensen PB, Nørgaard B, Waltoft BL. Toxoplasma gondii as a risk factor for early-onset schizophrenia: analysis of filter paper blood samples obtained at birth. Biol Psychiatry 2007; 61:688-93.
- Torrey EF, Bartko JJ, Lun ZR, Yolken RH. Antibodies to Toxoplasma gondii in patients with schizophrenia :a meta-analysis. Schizophr Bull 2007; 33:729-36.
- Sheehan D, Janavs J, Harnett-Sheehan K, Sheehan M, Gray C. Mini International Neuropsychiatric Interview (MINI) 2009 English version 6.0.0 DSM-IV.
- Hamidinejat H, Ghorbanpoor M, Hossein H. Toxoplasma gondii infection in first-episode and inpatient individuals with schizophrenia. Inter J Infec Dis 2010; 14:978-81.
- Yolken RH, Dickerson FB, Torrey EF. Toxoplasma and schizophrenia. Parasite Immunol 2009; 31:706-15.
- Amminger GP, McGorry PD, Berger GE. Antibodies to infectious agents in individuals at ultra-high risk for psychosis. Biol Psychiatry 2007; 61:1215-7.
- Schwarcz R, Hunter CA. Toxoplasma gondii and schizophrenia: linkage through astrocyte-derived kynurenic acid. Schizophr Bull 2007; 33:652–3.
- Alipour A, Shojaee S, Mohebali M, Tehranidoost M, Abdi MF.Toxoplasma infection in schizophrenia patients:A comparative study with control group. Iran J Parasitol 2011; 6:31-7.
- Emelia O, Amal RN, Ruzanna ZZ, Shahida H, Azzubair Z, Tan KS. Seroprevalence of anti-Toxoplasma gondii IgG antibody in patients with schizophrenia. Trop Biomed 2012; 29(1): 151-9.
- Saraei SM, Shamloo F, Jahani HH, Khabba F, Alizade SA. Relation between Toxoplasma gondii infections and schizophrenia. Iranian J Psychiatr Clin Psychol 2009; 15(1):3–9.
- Kozar Z. toxoplasmosis among the mentally sick. Bull Inst Med Mar Trop Gdansk.1953; 5:146-73.
- Dickerson F, Stallings C, Origoni A , Boronow J, Yolken R. C-reactive protein is associated with the severity of cognitive impairment but not of psychiatric symptoms in individuals with schizophrenia. Schizophr Res 2007; 93:261-6.
- Beverley JK, Fleck DG , Kwantes W. Age–sex distribution of various diseases with particular reference to toxoplasmic lymphadenopathy. J Hyg (Camb) 1976; 76:215–8.
- Akanji AO, Ohaeri JU, Al-Shammri S, Fatania HR. Association of blood levels of C-reactive protein with clinical phenotypes in Arab schizophrenic patients. J Phys 2009; 56-61.
- Fan X, Pristach C, Liu EY, Freudenreich O, Henderson DC, Goff DC. Elevated serum levels of C-reactive protein are associated with more severe psychopathology in a subgroup of patients with schizophrenia. Psychiatry Res 2007;149: 267–71.
- Mazzarello V, Cecchini A, Fenu G, Rassu M, Dessy LA, Lorettu L, et al. Lymphocytes in schizophrenic patients under therapy: serological, morphological and cell subset findings. Ital J Anat Embryol 2004; 109: 177–88.
- Diaz FJ, Iglesias PR, Mata I, Garcia OM. Possible effects of some antipsychotic drugs on C-reactive protein in a drug-naive psychotic sample. Schizophr Res 2010; 207-12
- de-Leon J, Dia Fj. Planning for optimal design of studies to personalize antipsychotic prescriptions in the post-CATIL era: the clinical and pharmacoepidemiological data suggest the pursuing the pharmacogenetics of metabolic syndrome complications (hypertension, diabetes mellitus and hyperlipidemia) may be a reasonable strategy. Schizophr.Res 2007: 96; 185-97.
- Meyer JM, Stahi SM. The metabolic syndrome and schizophrenia. Acta Psychiatr Scand 2009; 119:4-14.
How to Cite
Bakre, H. M., Hussain, S. K., & Ali, S. K. (2015). Toxoplasma gondii infection in patients with schizophrenia. Zanco Journal of Medical Sciences (Zanco J Med Sci), 19(1), 874_879. https://doi.org/10.15218/zjms.2015.0006